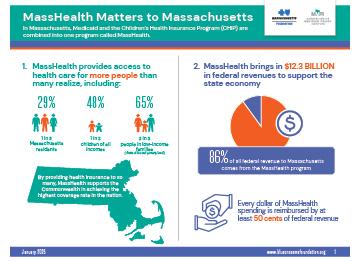
MassHealth, Massachusetts’ Medicaid and Children’s Health Insurance Program, is facing meaningful challenges as federal budget cuts threaten its stability and capacity to serve approximately 2 million residents. The program, which brings in around $15 billion in federal revenue to the state, is at a crossroads amid proposed reductions that could force challenging choices impacting care access and affordability for vulnerable populations. State officials and healthcare leaders are grappling with how to sustain critical coverage and support services in the face of shifting national policies and ongoing systemic pressures on the healthcare system [[3]](https://www.capecodtimes.com/story/news/state/2025/04/08/medicaid-trump-budget-cuts-ma-childrens-health-insurance-healey-walsh/82988335007/).
Table of Contents
- MassHealth Faces Funding Uncertainties as Federal Medicaid Policies Evolve
- Impact on Beneficiaries Highlights Need for Enhanced Outreach and Support
- State Officials Call for Strategic Adaptations to Maintain Coverage and Care Quality
- Experts Recommend Policy Reforms to Stabilize MassHealth Amid National Shifts
- Concluding Remarks
MassHealth Faces Funding Uncertainties as Federal Medicaid Policies Evolve
MassHealth is navigating a turbulent fiscal landscape as federal Medicaid policies undergo significant revisions. Recent changes at the federal level have introduced uncertainties about the future flow of funding, raising concerns among state officials charged with maintaining vital healthcare coverage for millions of Massachusetts residents. These adjustments potentially affect the allocation formulas and eligibility criteria that states rely on to manage program budgets, posing challenges to MassHealth’s capacity to sustain comprehensive services.
Stakeholders are closely monitoring developments that could impact:
- Funding stability amid shifting federal priorities
- Eligibility requirements and potential tightening of coverage standards
- Program administration and the ability to innovate service delivery
With evolving federal Medicaid guidelines, MassHealth faces pressure to adapt quickly while ensuring that vulnerable populations do not lose access to essential care. The state’s healthcare advocates emphasize the importance of maintaining robust support systems during this period of change to protect the health and well-being of its communities.
Impact on Beneficiaries Highlights Need for Enhanced Outreach and Support
The recent federal shifts in Medicaid policies have amplified the complexities faced by MassHealth beneficiaries, revealing significant gaps in awareness and access. Many applicants continue to experience delays in coverage activation,underscoring the critical need for faster,more clear dialog channels. Without timely support, vulnerable populations risk prolonged periods without essential healthcare services, exacerbating health disparities across the state. Frontline reports indicate confusion in navigating eligibility criteria and application processes, emphasizing that existing outreach efforts fall short in addressing the diverse needs of Massachusetts residents.
Key areas requiring immediate attention include:
- Enhancement of community-based outreach programs tailored to linguistically and culturally diverse populations.
- Investment in streamlined digital platforms and dedicated helplines to guide applicants through complex procedures.
- Training for local service providers to ensure comprehensive and empathetic assistance.
- Collaboration with social service agencies to proactively identify and support at-risk individuals before coverage lapses.
Collectively, these strategies aim to close the gap between policy intentions and real-world beneficiary experiences, fostering a more inclusive and efficient health coverage landscape in Massachusetts.
State Officials Call for Strategic Adaptations to Maintain Coverage and Care Quality
In response to ongoing federal Medicaid policy changes, Massachusetts state officials emphasize the urgent need for strategic adaptations within the MassHealth program to safeguard both coverage levels and care quality. Recognizing the potential risks posed by federal funding adjustments, officials advocate for a multi-faceted approach that includes:
- Strengthening partnerships with community health providers to ensure uninterrupted access
- Expanding use of innovative care delivery models to optimize resource allocation
- Enhancing data-driven oversight to swiftly identify gaps and adjust policies
State leaders also highlight the importance of proactive engagement with beneficiaries to navigate bureaucratic hurdles commonly encountered during transitions. By increasing accessibility through services like Mass211, which connects residents to essential resources including MassHealth enrollment assistance and related support agencies, Massachusetts aims to maintain a robust safety net amid evolving federal mandates.These coordinated efforts strive to minimize coverage disruptions while promoting equitable health outcomes for vulnerable populations statewide.
Experts Recommend Policy Reforms to Stabilize MassHealth Amid National Shifts
Amid evolving federal Medicaid regulations,health policy experts urge Massachusetts to implement targeted reforms to ensure the long-term viability of MassHealth. Key proposals emphasize improving administrative efficiency and fortifying funding mechanisms to counterbalance unpredictable federal budget shifts. Experts highlight the necessity of modernizing enrollment processes, aiming to reduce bottlenecks and provide quicker access to benefits for vulnerable populations. Equally critical is expanding partnerships with community organizations to streamline outreach, ensuring those newly eligible under federal changes are not left uninsured.
Recommended reforms include:
- Enhanced data integration systems for real-time eligibility verification
- Increased investment in provider reimbursement rates to maintain care quality
- Strengthening coordination between MassHealth and social services to address social determinants of health
- Greater versatility in state budget allocations to buffer against federal funding fluctuations
These strategic initiatives aim to build resilience within MassHealth, safeguarding access to healthcare amid national Medicaid policy shifts. Advocates stress the importance of legislative action that balances fiscal responsibility with equitable healthcare delivery, positioning Massachusetts as a leader in adaptive Medicaid program management.
Concluding Remarks
As MassHealth navigates these unprecedented federal Medicaid changes, the coming months will be critical in determining how effectively the program can adapt while continuing to serve Massachusetts’s vulnerable populations. Stakeholders remain watchful as policy shifts unfold, underscoring the importance of coordination between state and federal agencies to safeguard access to essential health coverage. The evolving landscape presents both significant challenges and opportunities for innovation in public health administration moving forward.